Prostatitisis an inflammatory disease of the prostate gland. Manifested by frequent urination, pain in the penis, scrotum, rectum, sexual disorders (erection dysfunction, early ejaculation, etc. ), sometimes urinary retention, blood in the urine. The diagnosis of prostatitis is established by a urologist or andrologist according to a typical clinical picture, the results of a rectal examination. Additionally, an ultrasound of the prostate, bakposev of prostatic secretion and urine is performed. Treatment is conservative - antibiotic therapy, immunotherapy, prostate massage, lifestyle correction.

General information
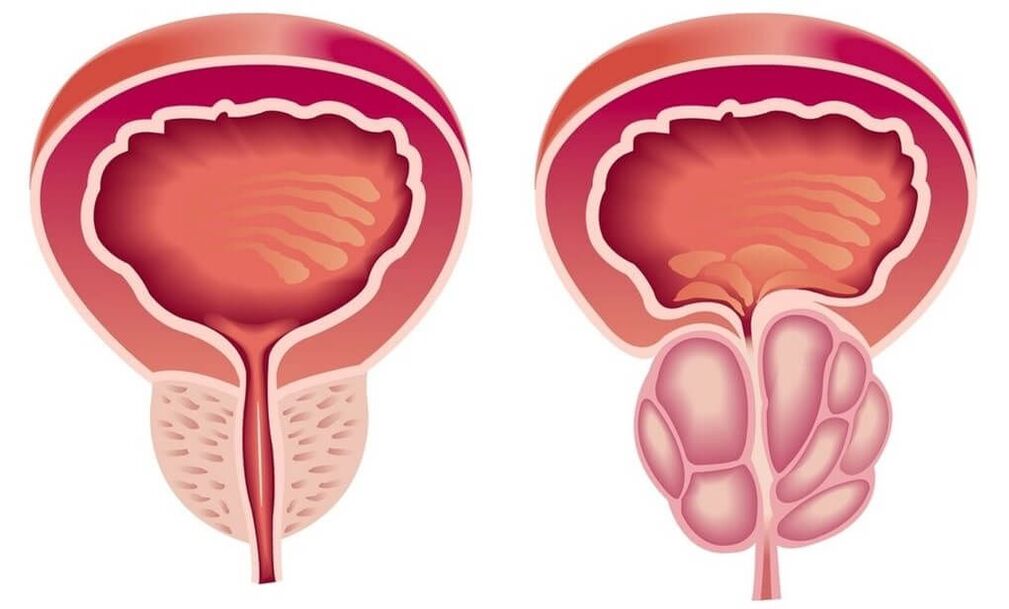
Prostatitis is an inflammation of the seminal (prostate) gland - the prostate. It is the most common disease of the genitourinary system in men. Most often affects patients aged 25-50 years. According to various data, 30-85% of men over the age of 30 suffer from prostatitis. Possible abscess formation of the prostate gland, inflammation of the testicles and appendages, which threatens infertility. The ascent of the infection leads to inflammation of the upper genitourinary system (cystitis, pyelonephritis).
Pathology develops with the penetration of an infectious agent that enters the prostate tissue from the organs of the genitourinary system (urethra, bladder) or from a distant inflammatory focus (with pneumonia, influenza, tonsillitis, furunculosis)
Causes of prostatitis
As an infectious agent in an acute process, Staphylococcus aureus (Staphylococcus aureus), Enterococcus (Enterococcus), Enterobacter (Enterobacter), Pseudomonas (Pseudomonas), Proteus (Proteus), Klebsiella (Klebsiella) and Escherichia coli (E. Coli) can act. Most microorganisms belong to conditionally pathogenic flora and cause prostatitis only in the presence of other predisposing factors. Chronic inflammation is usually due to polymicrobial associations.
The risk of developing the disease increases with hypothermia, a history of specific infections and conditions accompanied by congestion in the tissues of the prostate. There are the following predisposing factors:
- General hypothermia (one-time or permanent, associated with working conditions).
- A sedentary lifestyle, a specialty that forces a person to be in a sitting position for a long time (computer operator, driver, etc. ).
- Constant constipation.
- Violations of the normal rhythm of sexual activity (excessive sexual activity, prolonged abstinence, incomplete ejaculation during a "habitual" sexual intercourse devoid of emotional coloring).
- The presence of chronic diseases (cholecystitis, bronchitis) or chronic infectious foci in the body (chronic osteomyelitis, untreated caries, tonsillitis, etc. ).
- Past urological diseases (urethritis, cystitis, etc. ) and sexually transmitted diseases (chlamydia, trichomoniasis, gonorrhea).
- Conditions that cause suppression of the immune system (chronic stress, irregular and malnutrition, regular lack of sleep, overtraining in athletes).
It is assumed that the risk of developing pathology increases with chronic intoxication (alcohol, nicotine, morphine). Some studies in the field of modern andrology prove that chronic perineal trauma (vibration, concussion) in motorists, motorcyclists and cyclists is a provoking factor. However, the vast majority of experts believe that all of these circumstances are not the real causes of the disease, but only contribute to the exacerbation of the latent inflammatory process in the tissues of the prostate.
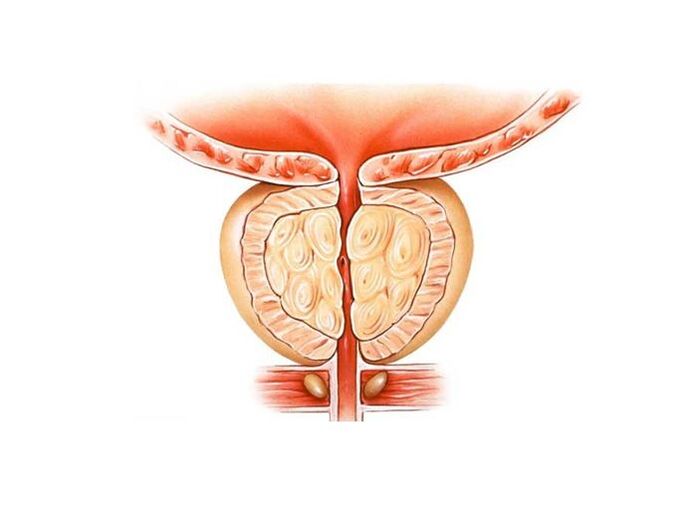
A decisive role in the occurrence of prostatitis is played by congestion in the tissues of the prostate. Violation of capillary blood flow causes an increase in lipid peroxidation, edema, exudation of prostate tissues and creates conditions for the development of an infectious process.
Symptoms of prostatitis
Acute prostatitis
There are three stages of acute prostatitis, which are characterized by the presence of a certain clinical picture and morphological changes:
- Acute catarrhal. Patients complain of frequent, often painful urination, pain in the sacrum and perineum.
- Acute follicular. The pain becomes more intense, sometimes radiating to the anus, aggravated by defecation. Urination is difficult, urine flows out in a thin stream. In some cases, there is urinary retention. Subfebrile condition or moderate hyperthermia is typical.
- Acute parenchymal. Severe general intoxication, hyperthermia up to 38-40°C, chills. Dysuric disorders, often - acute urinary retention. Sharp, throbbing pains in the perineum. Difficulty in defecation.
Chronic prostatitis
In rare cases, chronic prostatitis becomes the outcome of an acute process, however, as a rule, a primary chronic course is observed. The temperature occasionally rises to subfebrile values. The patient notes a slight pain in the perineum, discomfort during the act of urination and defecation. The most characteristic symptom is scanty discharge from the urethra during defecation. The primary chronic form of the disease develops over a considerable period of time. It is preceded by prostatosis (stagnation of blood in the capillaries), gradually turning into abacterial prostatitis.
Chronic prostatitis is often a complication of the inflammatory process caused by the causative agent of a specific infection (chlamydia, trichomonas, ureaplasma, gonococcus). Symptoms of a specific inflammatory process in many cases mask the manifestations of prostate damage. Perhaps a slight increase in pain during urination, mild pain in the perineum, scant discharge from the urethra during defecation. A slight change in the clinical picture often goes unnoticed by the patient.
Chronic inflammation of the prostate gland can be manifested by a burning sensation in the urethra and perineum, dysuria, sexual disorders, increased general fatigue. The consequence of violations of potency (or fear of these violations) often becomes mental depression, anxiety and irritability. The clinical picture does not always include all the listed groups of symptoms, differs in different patients and changes over time. There are three main syndromes characteristic of chronic prostatitis: pain, dysuric, sexual disorders.
There are no pain receptors in the prostate tissue. The cause of pain in chronic prostatitis becomes almost inevitable due to the abundant innervation of the pelvic organs, involvement in the inflammatory process of the nerve pathways. Patients complain of pain of varying intensity - from weak, aching to intense, disturbing sleep. There is a change in the nature of pain (intensification or weakening) with ejaculation, excessive sexual activity or sexual abstinence. Pain radiates to the scrotum, sacrum, perineum, sometimes to the lumbar region.
As a result of inflammation in chronic prostatitis, the volume of the prostate increases, squeezing the urethra. The lumen of the ureter is reduced. The patient has frequent urge to urinate, a feeling of incomplete emptying of the bladder. As a rule, dysuric phenomena are expressed in the early stages. Then compensatory hypertrophy of the muscular layer of the bladder and ureters develops. Symptoms of dysuria during this period weaken, and then increase again with decompensation of adaptive mechanisms.
In the initial stages, dyspotence may develop, which manifests itself differently in different patients. Patients may complain of frequent nocturnal erections, blurred orgasm, or worsening erections. Accelerated ejaculation is associated with a decrease in the threshold level of excitation of the orgastic center. Painful sensations during ejaculation can cause the refusal of sexual activity. In the future, sexual dysfunctions become more pronounced. At the advanced stage, impotence develops.
The degree of sexual disorder is determined by many factors, including the sexual constitution and the psychological mood of the patient. Violations of potency and dysuria can be due to both changes in the prostate gland and the suggestibility of the patient, who, if he has chronic prostatitis, expects the inevitable development of sexual disorders and urination disorders. Especially often psychogenic dyspotence and dysuria develops in suggestible, anxious patients.
Impotence, and sometimes the very threat of possible sexual disorders, is hard to tolerate by patients. Often there is a change in character, irritability, obnoxiousness, excessive concern for one's own health, and even "care for the disease. "
Complications
In the absence of timely treatment of acute prostatitis, there is a significant risk of developing a prostate abscess. With the formation of a purulent focus, the patient's body temperature rises to 39-40 ° C and can become hectic in nature. Periods of heat alternate with severe chills. Sharp pains in the perineum make it difficult to urinate and make defecation impossible.
The increase in prostatic edema leads to acute urinary retention. Rarely, an abscess spontaneously ruptures into the urethra or rectum. When opened, purulent, cloudy urine with an unpleasant pungent odor appears in the urethra; when opened, the feces contain pus and mucus in the rectum.
Chronic prostatitis is characterized by an undulating course with periods of long-term remissions, during which inflammation in the prostate is latent or manifests itself with extremely poor symptoms. Patients who are not bothered by anything often stop treatment and turn only when complications develop.
The spread of infection through the urinary tract causes the occurrence of pyelonephritis and cystitis. The most common complication of the chronic process is inflammation of the testicles and epididymis (epdidymo-orchitis) and inflammation of the seminal vesicles (vesiculitis). The outcome of these diseases is often infertility.
Diagnostics
The characteristic clinical picture simplifies the process of diagnosis in acute and chronic prostatitis. It is mandatory to:
Treatment of prostatitis
Treatment of acute prostatitis
Patients with an uncomplicated acute process are treated by a urologist on an outpatient basis. With severe intoxication, suspicion of a purulent process, hospitalization is indicated. Antibacterial therapy is carried out. Preparations are selected taking into account the sensitivity of the infectious agent. Antibiotics are widely used that can penetrate well into prostate tissues.
With the development of acute urinary retention against the background of prostatitis, they resort to installing a cystostomy, and not a urethral catheter, since there is a danger of the formation of an abscess of the prostate. With the development of an abscess, an endoscopic transrectal or transurethral opening of the abscess is performed.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should be complex, including etiotropic therapy, physiotherapy, immunity correction:
- Antibiotic therapy. The patient is prescribed long courses of antibacterial drugs (within 4-8 weeks). Selection of the type and dosage of antibacterial drugs, as well as determining the duration of the course of treatment is carried out individually. The drug is chosen based on the sensitivity of the microflora according to the results of urine culture and prostate secretion.
- Prostate massage.Massage of the gland has a complex effect on the affected organ. During the massage, the inflammatory secret accumulated in the prostate gland is squeezed out into the ducts, then enters the urethra and is removed from the body. The procedure improves blood circulation in the prostate, which minimizes congestion and ensures better penetration of antibacterial drugs into the tissue of the affected organ.
- Physiotherapy.To improve blood circulation, laser exposure, ultrasonic waves and electromagnetic vibrations are used. If it is impossible to carry out physiotherapeutic procedures, the patient is prescribed warm medicinal microclysters.
In chronic, long-term inflammation, an immunologist's consultation is indicated to select the tactics of immunocorrective therapy. The patient is given advice on lifestyle changes. Making certain changes in the lifestyle of a patient with chronic prostatitis is both a curative and a preventive measure. The patient is recommended to normalize sleep and wakefulness, establish a diet, conduct moderate physical activity.
For the treatment of prostatitis, antibiotic therapy is most effective. Phytotherapy, immunocorrectors and hormonal preparations can also be used as prescribed by a doctor.
In the absence of acute symptoms, prostatitis can be treated with physiotherapy methods. In case of abscesses and suppurations, surgical intervention is recommended.
Treatment with drugs
Treatment of prostatitis through antibiotic therapy should begin with bakposev, the purpose of which is to assess the body's sensitivity to this type of antibiotic. In violation of urination, a good result is the use of anti-inflammatory drugs.
Medicines are taken in tablets, in acute cases - in the form of a dropper or intramuscularly. For the treatment of chronic forms of prostatitis, rectal suppositories are effective: with their help, drugs reach their goal faster and have minimal effect on other organs.
Blood-thinning and anti-inflammatory drugs have also proven themselves well.
Antibacterial therapy
Antibiotics are an effective remedy in the fight against bacterial prostatitis. In order to achieve the desired effect and not harm the body, the choice of medicine, dosage and treatment regimen should be handled by a doctor. For the correct selection of the most effective drugs, he will have to find out which type of pathogen caused prostatitis, and also check the patient for tolerance to antibiotics of a particular group.
For the effective treatment of chronic prostatitis, antibiotics of the fluoroquinolone group have proven themselves well. Their action is aimed at suppressing a bacterial infection and strengthening the body's own immunity. In addition, a bacteriostatic antibiotic is recommended for the prevention and treatment of concomitant diseases of the genitourinary system.
Treatment of prostatitis caused by mycoplasma and chlamydia can be additionally carried out with macrolide and tetracycline drugs, which slow down the spread of infection.
The duration of taking antibacterial drugs is from 2 to 4 weeks. In case of positive dynamics, the course can be extended.
Physiotherapy
Physiotherapeutic methods in the treatment of prostatitis are aimed at activating blood circulation in the pelvic area, improving metabolic processes in the prostate gland, and cleansing the ducts. If physiotherapy is combined with taking antibiotics, then the effect of the latter is enhanced.
The main methods include:
- magnetotherapy;
- laser therapy;
- electrophoresis;
- warming up;
- ultrasound;
- mud treatment;
- high frequency irradiation;
- physiotherapy.
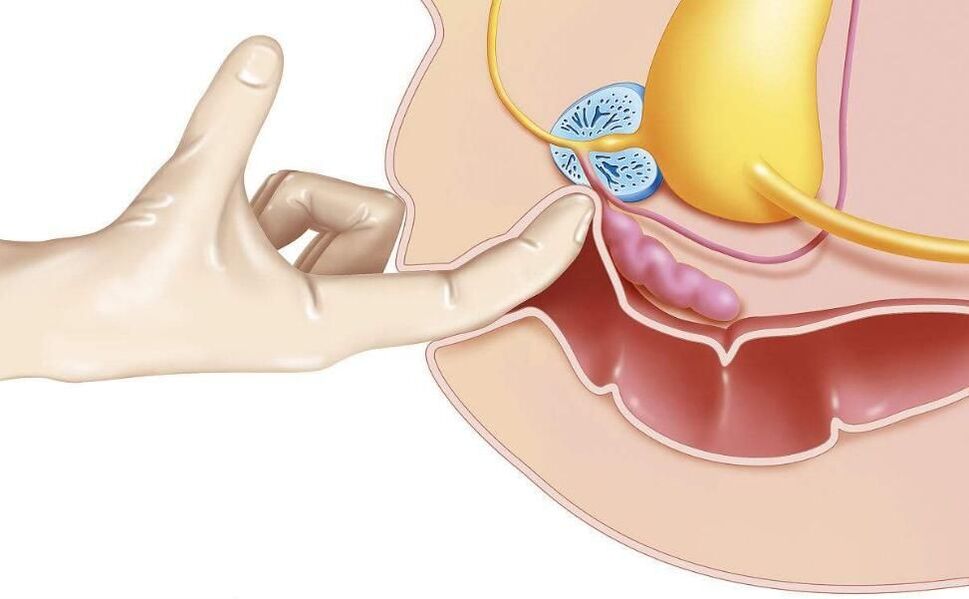
One of the oldest methods - transrectal prostate massage, according to modern research, has no proven effectiveness.
Non-specific treatments
Nonspecific treatments for prostatitis include:
- hirudotherapy;
- curative fasting;
- acupuncture;
- diet according to the method of Ostrovsky;
- alkalization of the body according to the method of Neumyvakin.
All non-traditional methods of treating prostatitis are strongly recommended to be coordinated with your doctor.
Surgery
Surgical methods are resorted to in complex and emergency cases:
- for drainage of purulent abscesses, which are removed by laparoscopic methods through a puncture;
- in violation of urination due to damage to the urinary tract;
- with a large volume of the affected area;
- with a significant number of stones in the body of the gland.
Stones and sclerosed tissues are removed by endoscopic methods. With a large area of damage or multiple stones, resection of the prostate is resorted to.
Transurethral resection is also effective for bacterial prostatitis. Thus, it is possible to reduce the risk of relapse.
Folk remedies
Treatment of prostatitis with folk remedies is unlikely to be effective on its own, but in combination with medical and physiotherapeutic methods it can be applicable. These include: beekeeping products, decoctions of herbs and seeds, tinctures of garlic, ginger, beaver stream, fresh vegetables, pumpkin seeds.
In acute cases of the course of the disease, you must consult a doctor, and in no case should you self-medicate! In case of rupture of a purulent abscess, a lethal outcome is possible.
Candles for prostatitis
Treatment of prostatitis with rectal suppositories is much more effective than tablets, if only because the rectum is much closer to the prostate, which means that the medicine will work faster.
The composition of drugs for the treatment of prostatitis can be completely different, they are prescribed to solve a particular problem.
- Antibacterial agents are especially effective for prostatitis caused by chlamydia.
- Painkillers are used for symptomatic treatment, they relieve pain well.
- Immunostimulants improve blood circulation, relieve swelling, and are used in complex therapy.
- Phytopreparations have a mild effect. They, like candles on bee products, are used as an addition to the main treatment.
- Compositions based on ichthyol promote blood flow in the area of the intestinal mucosa, which accelerates the attenuation of inflammatory processes and slightly improves immunity.
- Enzyme-based products prevent the formation of scar tissue. It is recommended to take as part of complex therapy with antibiotics, anti-inflammatory and analgesic drugs.
Auxiliary drugs
For symptomatic treatment of prostatitis in men, such as relief of pain during urination, you can additionally take antispasmodics that relax smooth muscles and thereby quickly relieve pain.
Blood-thinning and anti-inflammatory dietary supplements based on bee products, pumpkin seed oil, extracts from palm fruits contribute to general recovery.
Diet and lifestyle
For the treatment of prostatitis, a correct, balanced diet and a healthy lifestyle are very important. Food should not contain spicy, fried, salty, pickled foods. In the acute form, alcohol is strictly prohibited.
Food should contain enough fiber to prevent constipation. The protein content should be reduced. It is desirable to supplement the diet with herbs, ginger, pumpkin seeds.
Non-drug treatment
Non-drug methods of therapy allow you to act directly on the prostate, increase the concentration of drugs in its tissues, help eliminate congestion.
Microwave hyperthermia is performed using a rectal probe that is inserted into the patient's anus. On the device, you can set the temperature required for a particular type of exposure. To increase the concentration of the drug in the prostate requires heating 38-40°C. To obtain an antibacterial effect - 40-45 ° C.
Today, non-drug treatment focuses on laser therapy. The possibilities of this technique are wide. Under the influence of a laser, the following processes occur in the prostate gland:
- activation of redox reactions;
- improves blood microcirculation;
- new capillaries are formed;
- pathogenic microflora is suppressed;
- the process of cell division is activated, which contributes to tissue regeneration.
During the period of research into the effects of laser therapy on patients with prostatitis, a side effect, but positive for the purposes of treatment, was noticed. In those who completed the course, potency increased, erectile dysfunction was eliminated, and vitality was restored. To achieve this result, it is necessary to use a beam with a certain wavelength. In general, low-intensity laser radiation is used to treat chronic prostatitis.
Patients can, on their own initiative, undergo a course of laser therapy, if not prescribed by the attending physician.
Surgical treatment of chronic prostatitis
Chronic prostatitis does not pose a threat to the patient's life, but can significantly reduce its quality. The most serious complication of this disease is the formation of stones in the tissues of the gland. In order to free it from prostoliths, transurethral resection is used.
Surgery is carried out under the control of TRUS.
If complications such as prostate sclerosis occur, transurethral electrosurgery is performed. If, in combination with this pathology, sclerosis of the bladder neck is observed, a partial resection of the prostate is performed.
With blockage of the seminal and excretory ducts, endoscopic operations are indicated to eliminate violations of the patency of the secret. For this purpose, an incision is made in the seminal vesicles and excretory ducts. With an abscess, complete removal of the gland is possible.
Consequences of untreated prostatitis
Even if the symptoms of prostatitis do not appear for a long time, it is necessary to regularly undergo examination by a urologist. Not fully cured prostatitis may be accompanied by the formation of calcifications, which then have to be removed along with the gland. Experts are sure that there are no other ways to remove or dissolve stones.
In addition, pathogenic microorganisms can migrate to neighboring organs, causing inflammation. Running prostatitis can cause the development of adenoma and prostate cancer.
Forecast and prevention
Acute prostatitis is a disease that has a pronounced tendency to become chronic. Even with timely adequate treatment, more than half of the patients end up with chronic prostatitis. Recovery is far from always achieved, however, with correct consistent therapy and following the doctor's recommendations, it is possible to eliminate unpleasant symptoms and achieve a long-term stable remission in a chronic process.
Prevention is to eliminate risk factors. It is necessary to avoid hypothermia, alternate between sedentary work and periods of physical activity, eat regularly and fully. For constipation, laxatives should be used. One of the preventive measures is the normalization of sexual life, since both excessive sexual activity and sexual abstinence are risk factors in the development of prostatitis. If symptoms of a urological or sexually transmitted disease appear, you should consult a doctor in a timely manner.





























